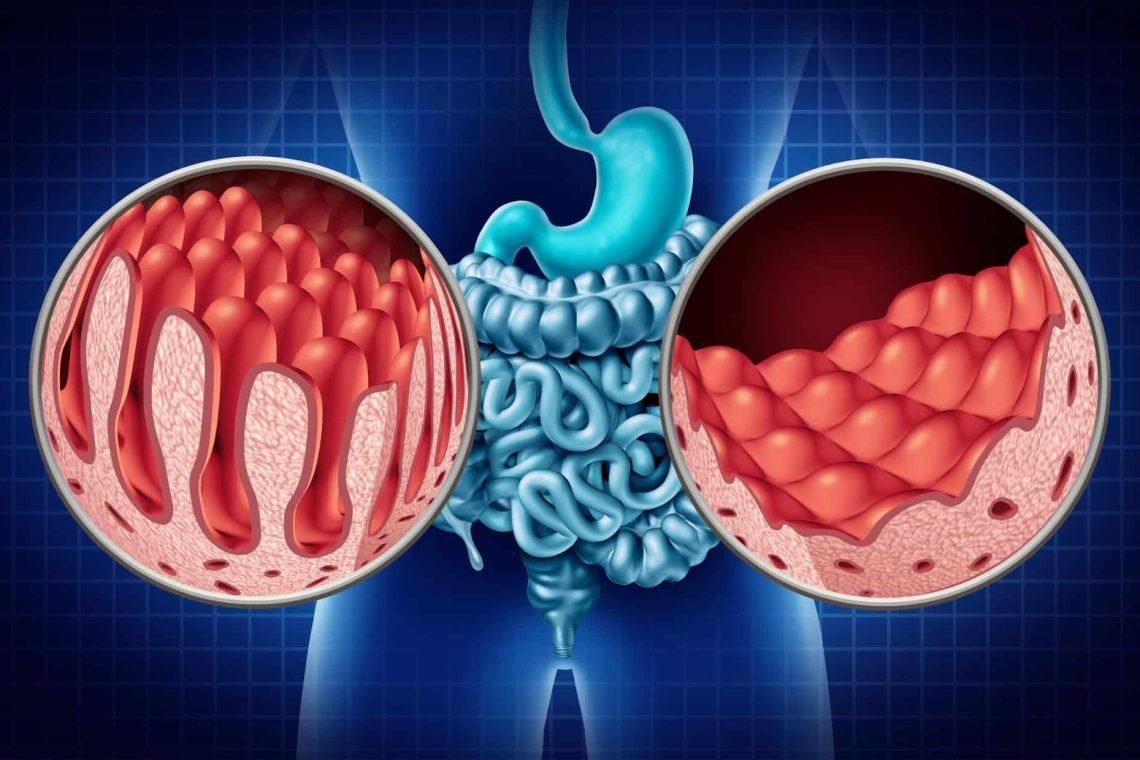
What is coeliac disease?
Coeliac disease is an auto-immunne disease. It is not a food allergy or intolerance to gluten. All those diagnosed with coeliac disease must follow a gluten free diet. Gluten is found in wheat, barley, rye, bulgar wheat, semolina, farina and spelt. For example bread, pasta, noodles, biscuits, cakes, breakfast cereals, beer, packaged soups/ sauces and even communion host.
It is not something people are born with but rather develop. Certain circumstances have been linked to the development of coeliac disease such as viral infections and weaning (too much or too little). However, there’s still lots of areas that reamin unknown.
It primarily affects the gut but doesn’t result in gut issues in nearly half of people. Please see a list of gut issues below. You may have some of them! As you can see, undiagnosed coeliac disease (or not following a strict gluten free diet when coeliac) can impact every inch of the body!
Symptoms
| Diarrhoea | Bloating | Constipation | Weight loss | Abdominal pain |
| Indigestion | Anxiety | Delayed puberty | Earlier menopause | Mouth ulcers |
| Short stature | Slow growth | Loss of tooth enamel | Osteoporosis | Low iron |
| Low vitamin B12 | Low vitamin D | Low folate | Fertility challenges | Migraine |
| Depression | Skin rash | Heart burn | Nausea | Lactose intolerance |
| Depression | Headaches | Tiredness | Exhaustion | ‘Brain Fog’ |
| Balance issues | Numbness | Coordination issues | Dermatitis Herpetiformis (1 in 10 people) | Hair loss |
Some stats
- 1.7 in 100 people have coeliac disease in Ireland
- 3 in 4 people do not know that they have coeliac disease.
- If you have a parent, child or sibling with coeliac disease, you have a 1 in 10 chance of having it developing it (but 80% of family members are not tested!)
- 2 in 5 people with undiagnosed coeliac disease have NO GUT ISSUES.
- 1 in 4 people with lactose intolerance actually have coeliac disease.
- 1 in 5 people with IBS have coeliac disease.
- 1 in 5 people have neurological symptoms
- 3 in 5 people will have gut symptoms
- Less than 1 in 10 people with Type 1 Diabetes and coeliac disease show gut symptoms.
When should you be tested for coeliac disease?
- If one of your immediates family has coeliac disease.
- IBS
- 24% of people with lactose intolerance have undiagnosed coeliac disease
- 40% of people with undiagnosed coeliac disease do not experience gut symptoms.
- 1 in 5 with undiagnosed coeliac disease have neurological symptoms.
- Osteoporosis, especially at a younger age or if male. WHen someone is diagnosed with coeliac disease as an adult, they will be referred for a DEXA/ DXA scan to check their bones.
- If you have repeated low iron (40% of people with repeated low iron levels will have coeliac disease), vitamin B12, vitamin D or folate levels
- Underactive thyroid
- Fertility challenges
- Psoriasis. Studies show that up to 14% of people with psoriasis also have coeliac disease. Most (73%) show improvement when they start a strict gluten free diet.
- Other conditions: Coeliac disease is linked with other conditions e.g. Type 1 diabetes (4-11%), Downs Syndrome (3-12%), Turners Syndrome (2-8.6%), Hashimoto’s Thyroiditis, Hyperthroid, Hair loss, Dealyed puberty, Early Menopause.
- 1 in 10 people with coeliac disease have Dermatitis Herpetiformis. It’s often presistent and super itchy (yellow blister and then scabs from scratching). It usually takes 2 years to resolve once following a strict gluten free diet.
- About 4-11% of people with Type 1 Diabetes will develop/ have coeliac disease. Kids should be screened for coeliac disease upon diagnosis and every year for 5 years, then every 2-3 years. Adults should be screen every 2-3 years. Generally about 10% of Type 1 diabetics complain of gut symptoms upon diagnoses which is less than the 60% of those without Type 1 diabetes. Check for coeliac disease every year for 5 years after diagnosis and then every 3 years afterwards.
- 30% (3 in 10) of people carry the genes for coeliac disease and its the same gene invovled with Type 1 diabetes and underactive thyroid (hashimotos).
Other Important Points
- At the onset of weaning, you may see food refusal, reduced appetite, faltered growth or weight loss, muscle wasting in arms and legs, irritable and listless as well as gut symptoms (vomiting, diarrhoea, constipation, bloated abdomen).
- In older kids you may still see food refusal, the child smaller than siblings, altered bowel habit (particularly constipation), abdominal pain.
- Psoriasis can improve on a GFD if coeliac.
- 5% (1 in 20) of people cannot have GF oats due to the avenin in oats. This number may be higher!
- Gluten contamination is 20 ppm which is equivalent to 20 seconds in 11 days. It’s difficult to manage, especially with kids.
- Important: If in Ireland, use the Irish list of foods suppled by the coeliac society each year rather than the UK list as they are different. Foods and brands change so look through your cuboards each year.
- There is an estimated 85,000 people in Ireland have CD. 60,000 are undiagnosed including 12,000 children.
Can We Prevent Coeliac Disease?
- ESPGHAN 2024:
- Breastfeeding doesn’t look like it protects againsts coeliac disease
- Diet during pregnancy unlikely to have an effect
- Higher gluten intake up to the age of 5 years may increase the risk of coeliac disease but there is no ‘safe’ dose recommended at present
Undiagnosed Coeliac Disease
As mentioned above, 3 in 4 people do not know they have coeliac disease. Undiagnosed coeliac disease can cause cancer, osteoporosis, fatigue & exhaustion, fertility challenges, severe nutrient deficiencies and nerve damage.
50% of people with coeliac disease have low iron levels when they are diagnosed while 41% have low vitamin B12 levels. This results in a whole host of symptoms, not just fatigue.
How do you get screeened for coeliac disease?
Talk to your GP about being screened for coeliac disease. It involves a blood test for IgA tTGA along with anti-EMA. If the test is negative or inconclusive but there are strong clinical indications, then test for IgA deficiency and then test IgG tTG.
- You must be eating gluten twice a day for 6 weeks prior to this blood test for the test to be accurate (some say 2 slices of bread (3g or more of gluten) each day for 14 days). Have a ‘go hard or go home’ attitude with it for best results! IgA tTGA levels will go back to normal if gluten is eliminated from the diet. You don’t want the test to be inaccurate because you haven’t consumed enough.
- The blood tests screens for coeliac disease rather than tests for it (diagnoses it). You may be sent for a scope where they take a biopsy.
Treatment
A life long, strict gluten-free diet. Avoid all gluten at all times. Please book in with a Registered Dietitian for guidance and a supplement protocol. Additionally, it is extremely helpful to join the The Coeliac Society. They provide a food list every year that checks ingredients and cross contamination. Only foods that are guaranteed to be gluten free make this list!
Please note, PAYE patients can claim back on certain foods. Keep shopping receipts and the food list for 4 years!
Blood Tests
Considering getting the following checked
- Check for anemia (FBC and ferritin), vitamin B12 and folic acid as well as low vitamin D and TFTs (thyroid function tests)
- IgA tTGA (under 3 years – more false negatives so may need to be retested)
- anti EMA
- tTG more than 10 times more than normal – then positive EMA test – enough for diagnosis in kids (no biopsy)
- In adults – need a biopsy to confirm
- You need to be eating gluten rich foods in the 6 weeks prior to testing
- Gluten challenge – need 10 to 15 g of gluten across 2-3 meals each day – looks like 2 slices of bread, 2 weetabix and 4 tablespoons of pasta each day