Childhood and teen obesity is a growing concern in Ireland and the UK, with significant implications for public health. In recent years, the prevalence of obesity among children and adolescents has continued to rise, leading to an increased focus on understanding and combating this issue.
1 out of 5 kids, at least, are living with food-related ill health.
Key Takeaways
| Topic | Summary |
| Prevalence | 1 in 5 children have overweight or obesity, with significant disparities among different demographics. |
| Contributing Factors | Socioeconomic factors, access to healthy foods, and lifestyle factors. |
| Health Risks | Obesity in children and teens leads to higher risks of non-communicable diseases like diabetes, heart disease, and cancer. |
| Prevention Strategies | Multi-sector approaches, including education, policy changes, and community programmes, are essential for effective prevention and management. |
| Future Projections | If current trends continue, a significant proportion of today’s children are at risk of obesity-related health issues in adulthood. |
Current Trends in Childhood and Teen Obesity
Recent data indicates that nearly 1 in 5 children and adolescents in Ireland have overweight or obesity. This trend is not uniform across all demographics; certain groups, particularly those from lower socioeconomic backgrounds, are disproportionately affected. Every child, no matter where they live, should have the same opportunities to thrive and that starts with healthy food, adequate hydration and regular exercise.
Weight Status
- DEIS schools: 18.3% with overweight and 7% with obesity
- Non-DEIS schools: 12.6% with overweight and 3.5% with obesity
- On average, 6 primary school children in a classroom of 30 living with overweight or obesity
Improvements
- Most schools are free from food and drink advertisement and vending machines
- Sugar sweetened beverages are not available in most schools
- All schools teach nutritional education and have PE
Contributing Factors
Childhood and teen obesity in Ireland and the UK is influenced by a complex interplay of factors. Understanding these contributing factors is essential for developing effective interventions.
Socioeconomic Disparities
Socioeconomic status plays a significant role in childhood obesity. Families from lower-income backgrounds often have limited access to healthy foods and safe environments for physical activity. These communities might face food deserts, where affordable and nutritious food options are scarce, leading to higher consumption of processed and high-calorie foods (e.g. UPF).
Lifestyle Changes
The modern lifestyle, characterised by increased screen time and sedentary activities, has significantly impacted children’s physical activity levels. Most kids spend at least 3 hours a day watching TV. When you add in video games, tablets, phones etc… this increases to about 5 to 7 hours a day.
Ideally kids and teenagers would be doing 60 minutes of cardio or aerobic exercise per day (420 minutes each week). Only 1 in 4 children are reaching this target.
Globally, physical inactivity is thought to be responsible for:
- 6% of the burden of disease from coronary heart disease (Europe 6%; Ireland 9%)
- 7% of type 2 diabetes (Europe 7%; Ireland 11%)
- 10% of breast cancer (Europe 9%; Ireland 15%)
- 10% of colon cancer (Europe 10% ; Ireland 16%)
Dietary Habits
Dietary habits have shifted towards higher consumption of fast food (UPF) and sugary beverages. Marketing strategies targeting children often promote unhealthy food choices, contributing to poor dietary habits. Additionally, busy family schedules can lead to reliance on convenient, processed foods (UPF) rather than home-cooked meals.
Health Risks Associated with Childhood Obesity
The health risks associated with childhood and teen obesity are both immediate and long-term, affecting physical, psychological, and social well-being.
Physical Health Risks
Children with obesity are at an increased risk of developing type 2 diabetes, high blood pressure, and cardiovascular diseases at a younger age. The excess fat tissue places additional strain on the body’s systems, leading to conditions that were once considered adult diseases. For example, Type 2 Diabetes in childhood has become increasingly prevalent throughout the world. Research suggests that in Ireland 2% of children and adolescents with diabetes aged < 16 years had type 2 diabetes. All were overweight or obese and the average age at presentation was just under 13 years. 85% of these children also had additional complications like high blood pressure.
Psychological and Social Impacts
Obesity can significantly impact a child’s mental health. Children with obesity are more likely to experience low self-esteem, depression, and anxiety due to stigma and bullying. These psychological effects can further contribute to unhealthy eating behaviours and sedentary lifestyles, creating a vicious cycle.
Long-term Consequences
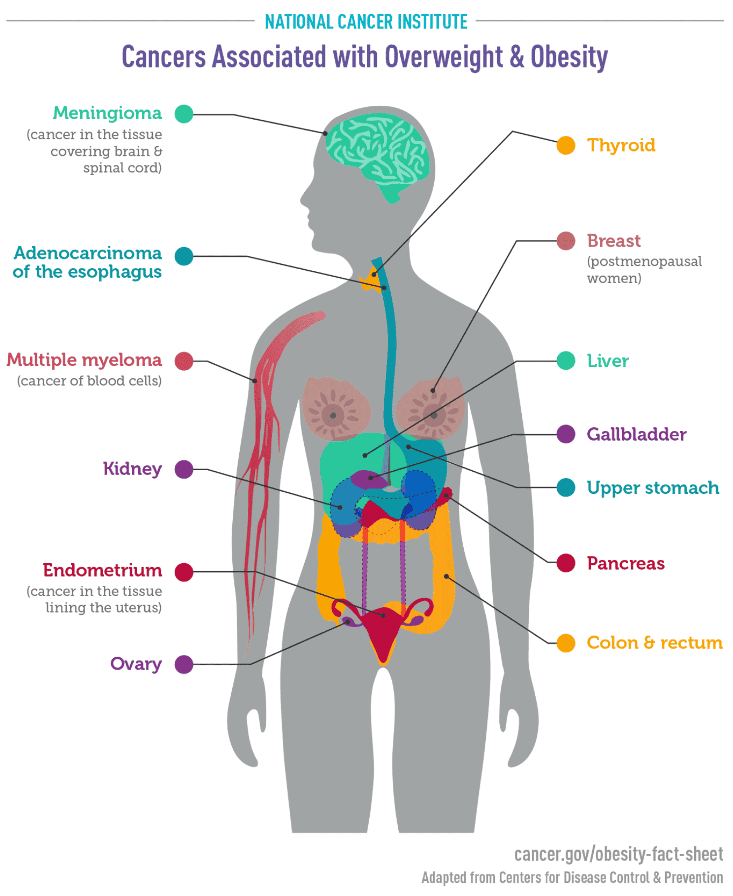
The long-term consequences of childhood obesity extend into adulthood. Children with obesity are more likely to become obese adults, continuing to face health risks such as heart disease, stroke, and certain cancers. For example, those with overweight or obesity are at increased risk of the 13 cancers listed below. This increase risk is signficiant e.g. endometrial cancer is 2–4 times as likely in people with obesity or overweight.
Prevention and Management Strategies
Addressing childhood and teen obesity requires a comprehensive approach that involves multiple sectors and stakeholders.
Policy Interventions
Effective policy interventions can create environments that promote healthy lifestyles. These policies may include:
- Nutritional Guidelines for Schools: Implementing and enforcing nutritional guidelines for schools to ensure children have access to healthy, balanced diets.
- Effective Education of Parents: With parenting there are so many things to consider. It’s hectic. Nutritional education has to be practical, consider costs and easy to implement even if time poor.
- Taxation on Sugary Beverages: This has lead to a drop in sugar content and reformulation of many drinks.
- Regulating Food Marketing: Restricting marketing of unhealthy foods to children to reduce their influence on dietary habits. Less healthy foods should not be at eye level for kids in the supermarket and should not have cartoons, animals etc on them.
- Provide fruit and vegetables in schools. Kids should have access to fresh water, fruit and vegetables in schools. Our kids environments are flooded with less healthy foods and drinks. We need to increase the flow of healthier options.
Community Programmes
Community-based programmes are essential in promoting healthy behaviours and providing support to families. Examples include:
- Healthy Eating Workshops: Conducting workshops that educate families on preparing nutritious meals and pulling mindsets towards a more wholefood approach. It shouldn’t be presumed that all adults know how to boil potatoes, an egg etc…
- Physical Activity Initiatives: Organising community sports events and creating safe spaces for children to engage in physical activities.
Educational Campaigns
Public health campaigns are vital in raising awareness about the importance of healthy eating and physical activity. These campaigns can:
- Promote Balanced Diets: Highlight the benefits of a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. The advice is the same whether overweight or not.
- Encourage Active Lifestyles: Emphasise the importance of regular physical activity and provide practical tips for incorporating exercise into daily routines. Again, the advice is the same whether overweight or not.
- Dispel Myths: Address common misconceptions about overweight and obesity.
Practical Steps for Parents and Guardians
Parents and guardians play a vital role in preventing and managing childhood obesity. Here are some practical steps that can be taken:
Encouraging Healthy Eating Habits
- Balanced Diets: Ensure children consume a balanced diet that includes a variety of fruits, vegetables, whole grains, and lean proteins.
- Portion Control: Teach children about listening to their body’s cues. In order to do this, mindful eating needs to be taught. For example, no screen time or TV at mealtimes.
- Family Meals: Eating together as a family can promote healthier eating habits and provide opportunities to introduce nutritious meals. This may not always be possible with evening sports and activities I know, but should be implemented when you can e.g. at breakfast time, Sunday lunch.
Promoting Physical Activity
- Active Play: Encourage children to engage in physical activities they enjoy, such as sports, dancing, or cycling. Aim for at least 60 minutes of moderate to vigorous physical activity each day.
- Limit Screen Time: Reduce the amount of time children spend on screens, including television, computers, and mobile devices. Encourage outdoor play and other physical activities instead.
- Incorporate Activity into Daily Routine: Simple activities like walking or cycling to school need to be a focus. Over 50% of journies taken in a car are for distances less than 2km.
Creating a Supportive Environment
- Positive Reinforcement: Praise and encourage children for making healthy choices and participating in physical activities.
- Lead by Example: Children are more likely to adopt healthy habits if they see their parents and guardians practicing them. Avoid talking negatively about your body image around your kids. Instead focus on what your body can do.
- Educational Resources: Utilise resources provided by schools, healthcare providers, and community programmes to stay informed about healthy lifestyle choices.
New recommendations for each age group include:
Infants aged less than a year should:
- be physically active several times a day in a variety of ways, particularly through interactive floor-based play
- not be secured for more than 1 hour at a time (e.g., prams/strollers, high chairs, or strapped on a caregiver’s back)
- Have 14–17h (0–3 months of age) or 12–16h (4–11 months of age) of good quality sleep, including naps.
Children aged 1-2 years should:
- spend at least 3 hours in a variety of physical activities at any intensity, spread throughout the day
- not be secured for more than 1 hour at a time (for example: prams/strollers, high chairs, or strapped on a caregiver’s back) or sit for extended periods of time
- Have 11-14 hours of good quality sleep, including naps, with regular sleep and wake-up times.
Children aged 3 – 4 years should:
- spend at least 3 hours in a variety of physical activities at any intensity, of which at least 1 hour is moderate-to vigorous-intensity physical activity, spread throughout the day
- not be secured for more than 1 hour at a time (e.g., prams/strollers) or sit for extended periods of time
- Have 10–13h of good quality sleep, which may include a nap, with regular sleep and wake-up times.
Children and adolescents aged 5-17 years, including those living a disability should:
- at least an average of 1 hour per day of moderate-to vigorous-intensity, mostly aerobic, physical activity, across the week
- additional activities that strengthen muscle and bones, should be incorporated at least 3 days a week
Conclusion
Addressing childhood and teen obesity in Ireland and the UK requires a concerted effort from policymakers, healthcare providers, communities, and families. It takes a village! By implementing comprehensive strategies that promote healthy eating, physical activity, and supportive environments, we can help ensure a healthier future for our children and adolescents.
FAQ on Childhood and Adolescent Obesity
What is the cause of childhood and adolescent obesity?
Childhood and adolescent obesity is caused by a combination of factors including genetics, lifestyle, and environment. Key contributors are unhealthy diets high in calories, sugar, and fats (usually due to high intakes of UPF, and low intakes of wholefoods); lack of physical activity; and socio-economic factors such as limited access to healthy foods and safe places for physical activity. The increasing availability of fast food and sugary snacks, combined with sedentary lifestyles, significantly contribute to rising obesity rates.
What age group is most affected by childhood obesity?
Depending on the criteria used, 11%-40% of children had overweight or obesity at 9 months, 14%-46% at 3 years and 8%-32% at 5 years of age. Almost one in ten (9%) of 3 year olds in lower socio-economic groups are obese compared with one in twenty (5%) in higher socio-economic groups.
Adults: Whilst men are more likely to be overweight than women (men: 43%, women: 31%), the proportions that are obese are more closely aligned (men: 25%, women: 22%). A smaller difference exists between men and women aged under 25 than those older than this. 31% of men aged 15-24 are overweight or obese, compared to 27% of women of this age. Women who are overweight or obese are more likely to be trying to lose weight than men who are overweight or obese.
How does puberty affect childhood obesity?
Puberty can influence obesity through hormonal changes that affect body fat distribution and metabolism. Additionally, puberty is a time of increased appetite and changes in physical activity patterns, which can lead to weight gain. In females, evidence suggests participation plummets during adolescence with just 7% of girls age 14-15 years meeting recommended physical activity levels.
What is obesity during childhood influenced by?
Childhood obesity is influenced by a range of factors including diet, physical activity, family habits, and broader social and environmental contexts. Unhealthy eating patterns and sedentary behaviours are significant contributors, alongside genetic predispositions and socio-economic conditions.
What is the biggest influence on childhood obesity?
The biggest influence on childhood obesity is a high intake of Ultr Processed Food rather than wholefoods and this is compounded by physical inactivity and sedentary behaviours which are influenced by excessive screen time.
Should parents be responsible for childhood obesity?
While parents play a crucial role in shaping their children’s eating and activity habits, childhood obesity is a complex issue influenced by many factors beyond parental control, including genetics, socio-economic status, and environmental factors. Thus, addressing obesity requires a holistic approach involving families, schools, communities, and policy interventions.
What is the strongest predictor of childhood obesity?
There are many predictors of childhood obesity. For example, how much time they spend sedentary, how much time they spend outdoors, their BMI at age 5, maternal diet, weight and behaviours (this will likely change over time due to the change in generalised societal roles).
Why is childhood obesity getting worse?
Childhood obesity is impacted by various factors, including increased availability and marketing of high-calorie, low-nutrient foods (typically UPF); sedentary lifestyles driven by screen time; and socio-economic inequalities that limit access to healthy food and safe recreational spaces. The COVID-19 pandemic may have exacerbated these trends by reducing physical activity opportunities and increasing reliance on processed foods.
What gender is most affected by childhood obesity?
Weight status by gender (in first class in school):
Bots: 8.5% thin, 75% healthy weight, 12.6% overweight and 3.9% obese.
Girls 8.8% thin, 72.4% healthy weight, 14.5% overweight and 4.3% obese.
Is childhood obesity due to bad parenting?
No! Absolutely not. There are so many different things that contribute to the weight and fat levels of a human body. Parents should not blame themselves and people should not blame parents.
Can you outgrow childhood obesity?
The rate of growth reduces considerably from age 1. Weight increases by 1.6 to 3.9kg per year after. They grow about 5 to 9 cm a year, slower in later childhood. However, they can have a major growth spurt later due to puberty. Body proportions of younger children change. Head growth is minimal and their trunk grows much slower. Their limbs lengthen a lot. Their legs straighten out due to movement and exercise. They lean up gradually, with lots of fat tissue as babies to quite lean bodies by age 4y. They’re typically at their leaness between 4 to 6 years, filling out at a later date leading up to puberty. From age 6 years the differnce in body fat levels and muscle mass start to show between boys and girls. When puberty hits the difference growns again. Girls generally increase their rate of weight gain between 10-11 years the most, while boys age 11-12 years which signals the approach of puberty.
How to reduce child obesity?
Reducing child obesity involves multiple strategies:
- Healthy Eating: Encourage balanced diets with plenty of fruits, vegetables, whole grains, and lean proteins. Limit sugary drinks and highly processed foods (foods you couldn’t make in your kitchen).
- Physical Activity: Promote at least 60 minutes of moderate to vigorous physical activity daily.
- Education: Educate families about healthy lifestyle choices.
- Policy Interventions: Implement policies that promote healthy eating and physical activity in schools and communities.
- Community Support: Provide community programmes that support healthy behaviours
How can local governments support the fight against childhood obesity?
Local governments can support the fight against childhood obesity by implementing policies that promote healthy lifestyles. This includes zoning regulations to limit the number of fast-food outlets near schools, creating safe and accessible recreational areas, and supporting local food initiatives that provide fresh, affordable produce. Additionally, local governments can fund community programs that educate families about nutrition and physical activity .
What role does genetics play in childhood obesity?
Genetics can influence a child’s susceptibility to obesity. Children with a family history of obesity are more likely to be obese themselves due to inherited traits that affect metabolism, fat storage, and appetite regulation. However, genetics is just one piece of the puzzle; lifestyle and environmental factors also play crucial roles in determining a child’s weight. Think of genetics being the gun, but environment pulls the trigger.
How effective are school-based interventions in reducing childhood obesity?
School-based interventions can be highly effective in reducing childhood obesity. These interventions include implementing nutritional standards for school meals, incorporating regular physical activity into the curriculum, and providing education on healthy eating and active living. Studies have shown that comprehensive school programs that combine these elements can significantly reduce obesity rates among students.
What are the psychological effects of childhood obesity?
Childhood obesity can have profound psychological effects, including low self-esteem, depression, and anxiety. Children who are obese are often subjected to bullying and social isolation, which can further impact their mental health. The body neutrality movement is having a positive impact on this, however, the movement needs to be better supported and moved forward at a faster pace.











